Fertility Treatment
Ballarat IVF is Regional Victoria’s only full time fertility service. Located in Ballarat, Ballarat IVF is easily accessible by couples from Geelong and greater Melbourne, as well as those from Western Victoria.
Overview
Ballarat IVF Fertility group Specialists provide a holistic fertility service, including General Gynaecological Fertility treatments and Specialist Assisted Reproduction treatment.
General Gynaecology Fertility treatments:
- In Person Medical Consultation, Assessment and Advice
- Easily accessed Telemedicine Consultation for fertility advice
- Diagnostic Ultrasound for endometriosis, adenomyosis, fibroids
- Diagnosis, treatment and Support for women with PCOS
- Fertility Nurse Email support
- Advanced Laparoscopic Surgery for Endometriosis fibroids and tubal disease
- Advanced, team based Treatment for Bowel Endometriosis
- Referrals for Fertility related Bariatric Surgery
- Referrals for Natural Fertility Therapy
- Counselling and Psychology Support
Specialist Assisted Reproductive Techniques (ART):
- Ovulation Induction, IUI (Intrauterine Insemination)
- IVF (In-Vitro Fertilisation), ICSI (Intra-Cytoplasmic Sperm Injection)
- Freezing and Storage of Embryos , Sperm, Eggs
- Semen Analysis
- Testicular Needle Biopsy, Sperm Retrieval Techniques (PESA)
- Donor Programs, for Eggs, Sperm, and Embryos
Treatments for Women
Treatments for Men
Results
We are often asked, “what are my chances of having a baby with Fertility treatment, or IVF?". This is a difficult question to answer accurately, as every couple’s circumstances, and the factors contributing to their infertility, differ. To state the obvious, every woman, and/or couple we see have a “fertility problem”, and often have a number of issues, contributing to their lack of success in conceiving. A person’s individual success rate may be affected by numerous factors, such as age, lifestyle factors (including weight and smoking), genetic factors and direct causes of infertility.
The best reference points to use are age related break downs of success rates, and to “overlay” this information with your fertility specialist’s assessment of your circumstances.
When an IVF unit, or group of Units report, or publish results, the information presented can often be difficult to apply to individual patients or couples.
Most comparisons between IVF services refer to Clinical Pregnancy Rates. A “clinical pregnancy” is defined as a pregnancy sac in the uterus, a miscarriage, an ectopic pregnancy, or, an ongoing viable pregnancy. What really matters is the live birth rate per episode of treatment, or course of treatment
It is important to note that not every treatment cycle will result in an egg collection, embryo transfer or have any embryos suitable for freezing. The likelihood of getting pregnant with a particular treatment is very important. This will be discussed with you during one of your fertility appointments.
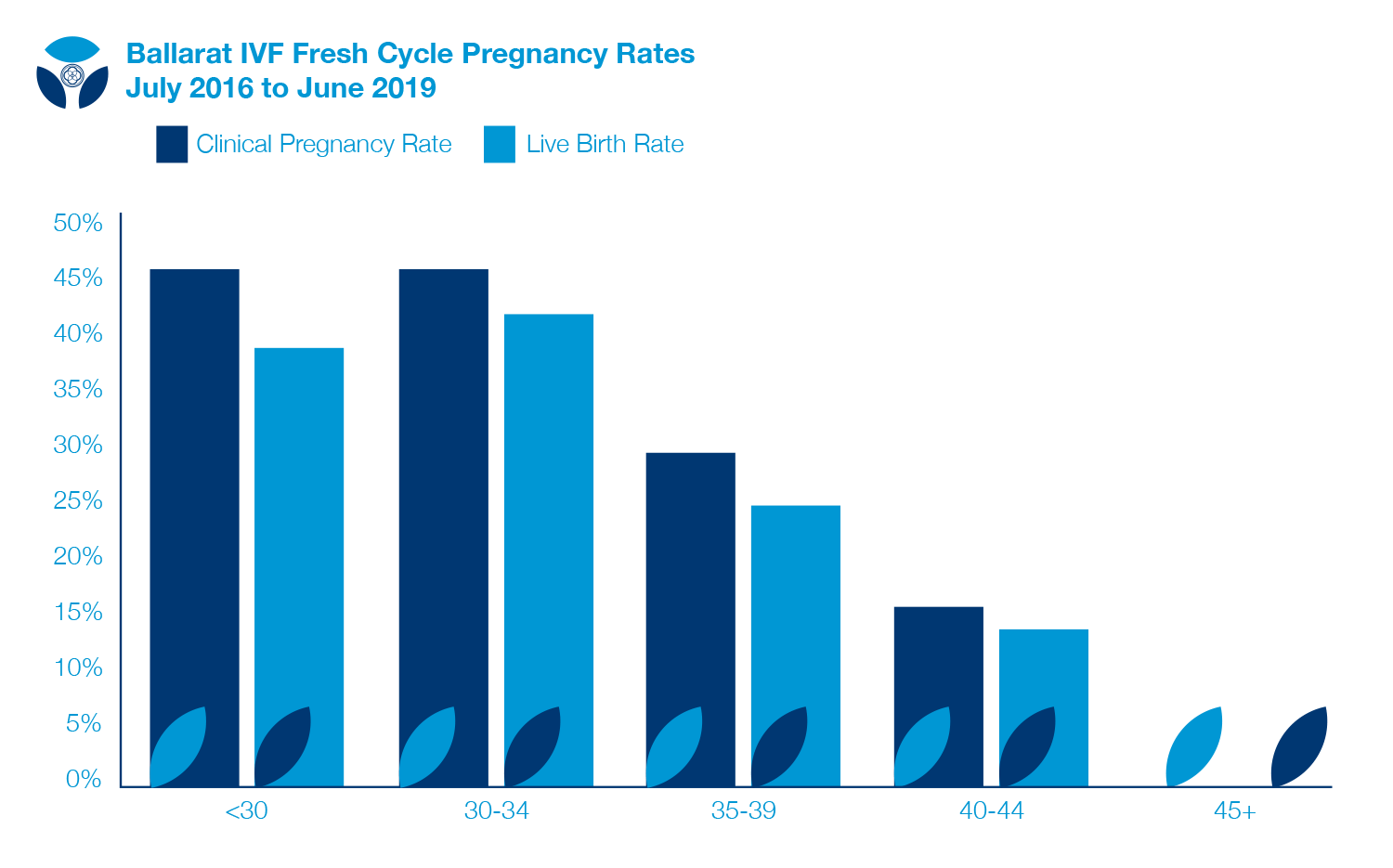
CYCLE TYPE Fresh OPU (ALL)
EMBRYO TYPE ALL
DATE RANGE July 2016 to June 2019
| <30 | 30-34 | 35-39 | 40-44 | 45+ | |
|---|---|---|---|---|---|
| No. Cycles | |||||
| Ets | 41 | 85 | 100 | 43 | 1 |
| Clinical Pregnancies | 19 | 39 | 30 | 7 | 0 |
| Live Births | 16 | 36 | 25 | 6 | 0 |
| Still Births | |||||
| Clinical Pregnancy Rate | 46% | 46% | 30% | 16% | 0% |
| Live Birth Rate | 39% | 42% | 25% | 14% | 0% |
For further information, visit the Your IVF Success Website: https://yourivfsuccess.com.au/clinics/116?term=&page=0&size=20&locationId=5903
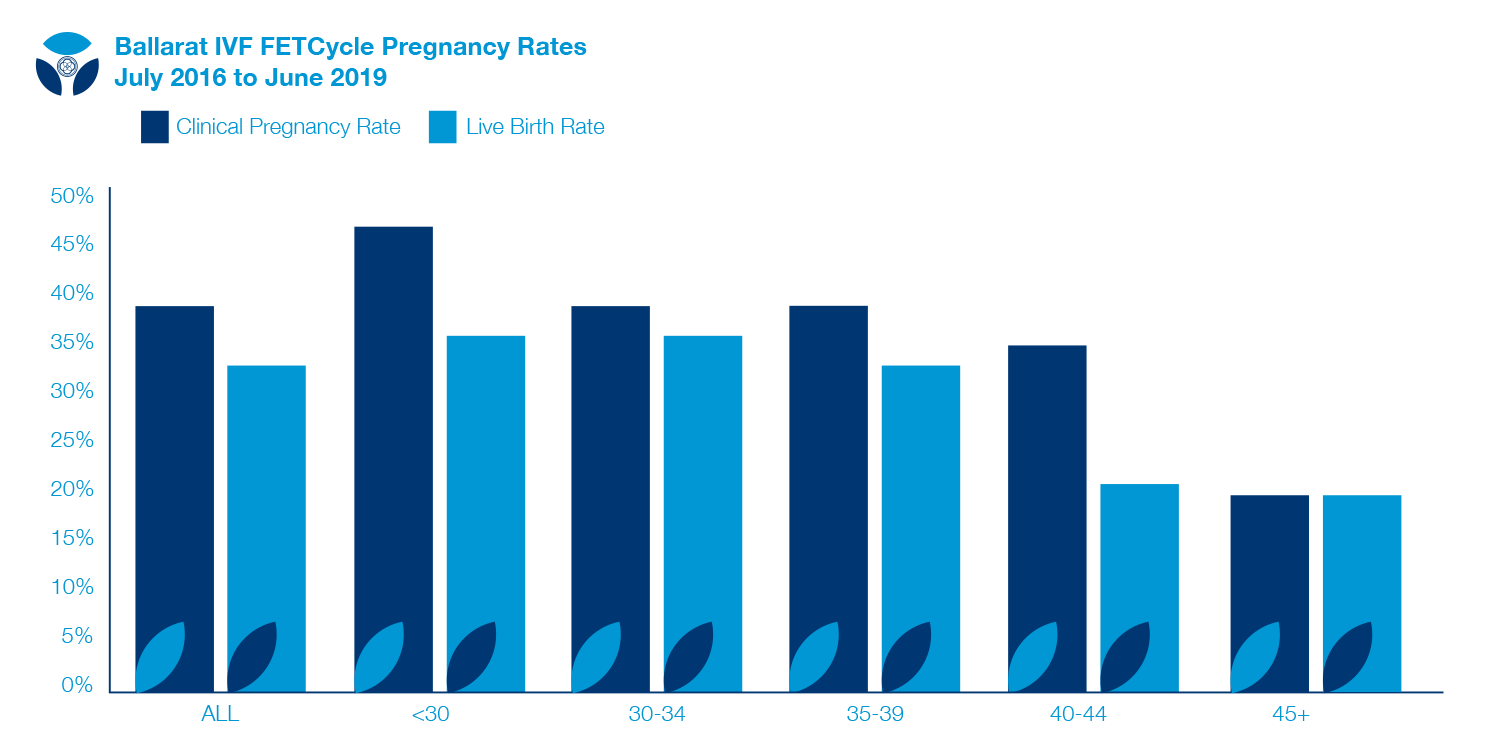
CYCLE TYPE FET
EMBRYO TYPE ALL
DATE RANGE July 2016 to June 2019
| All | <30 | 30-34 | 35-39 | 40-44 | 45+ | |
|---|---|---|---|---|---|---|
| No. Cycles | ||||||
| Ets | 714 | 100 | 253 | 259 | 92 | 10 |
| Clinical Pregnancies | 282 | 47 | 99 | 102 | 32 | 2 |
| Live Births | 234 | 36 | 91 | 86 | 19 | 2 |
| Still Births | ||||||
| Clinical Pregnancy Rate | 39% | 47% | 39% | 39% | 35% | 20% |
| Live Birth Rate | 33% | 36% | 36% | 33% | 21% | 20% |
Ovulation Induction (OI)
Infrequent ovulation is the most common cause of not getting pregnant. We are experts in providing Ovulation induction services.
We provide face to face Ovulation Induction, or Ovulation Induction Online through our world first AI program, OVUNET .
Ovulation induction is straight forward and affordable.
Ovulation induction involves:
- Registering with OVUNET or
- Having a Specialist consultation, which can be through telemedicine
- Taking letrozole to stimulate your ovaries
- Having an Ultrasound to assess your response
- Support and advice from your Fertility Nurse or OVUNET
- Testing your urine for an LH surge
- Having a trigger injection.
- Trying to conceive naturally.
Success rates:
Based on our own results, after 4 ovulation induction cycles, 33% of women will achieve a pregnancy, and 26% achieve a live birth.
Risk of ovulation induction:
Multiple birth. At Ballarat IVF 2-3% of Ovulation induction pregnancies are twins.
If your ovaries have more than 2 follicles, we will ask you not to try to conceive in that cycle.
Intrauterine Insemination (IUI) & Donor Insemination (DI)
This treatment involves the woman undertaking an Ovulation induction treatment cycle, then placing sperm into the uterine cavity at the time of ovulation.
Sperm may be from a woman’s male partner, or from a donor
Sperm is specially prepared by our IVF Scientists to select out the most motile sperm from the semen sample. This process takes 3 to 4 hours.
The IUI / Di procedure is performed in a similar way to a pap smear, without the need for anaesthetic
In Vitro Fertilisation (IVF)
For this treatment, eggs are collected from the woman, and combined with prepared sperm from a man in a micro drop of special nutrient media and held in an incubator.
Sperm naturally fertilise the egg. Embryo development is then observed by our scientists, and an embryo is transferred back to the woman 5 days later.
There are a number of steps to follow during IVF treatment:
1. Fertility Specialist Consultation – can be via Telehealth
2. Pre-Treatment Tests and Preparation
3. Fertility Specialist prescribes your personal treatment regimen
4. You give yourself FSH injections and some other medications
5. Ultrasound to monitor your response and Follicle Growth
6. You give yourself a trigger injection to mature the eggs on advice from your fertility nurse
7. Semen Collection or Donor Sperm preparation
5. Egg collection ( a day case procedure under sedation anaesthesia)
7. Insemination, Fertilisation and Embryo Culture
8. Embryo Transfer (ET) (carefully performed under Ultrasound guidance)
9. Embryo Freezing (of additional embryos)
10. Pregnancy Testing
Intra-Cytoplasmic Sperm Injection (ICSI)
ICSI treatment is a method of sperm micro-injection where a single sperm is injected into an egg.
It may used for couples who…
- have not been able to achieve fertilisation using routine IVF methods
- have semen test results that show that routine IVF is unlikely to give satisfactory results
- have had a vasectomy or reversal,
- have absent or blocked vas deferens (the tube that carries the sperm from the testicles)
DuoStim Treatment
What is DuoStim?
Duostim involves having a normal IVF stimulation regimen using FSH ( fertility drugs), having an egg collection procedure, then 5 days later, starting a new IVF stimulation cycle to re-stimulate your ovaries to produce a new group of mature eggs.
How does this happen?
During a normal IVF stimulation cycle, a group of follicles and oocytes are stimulated to grow, and are collected when they are mature. It is now understood that behind these mature eggs are a further group of eggs which have also been recruited by the fertility drugs, but are still small and immature. If we re-treat the woman with fertility drugs, this second wave of follicles and eggs will respond, grow, and mature, being ready for another egg collection in a short space of time.
Who needs DuoStim?
Women who don’t produce many eggs from their first egg collection will benefit from DuoStim. DuoStim gives the woman the opportunity to go straight back into a treatment plan, avoiding unnecessary delays, especially in older women.
Women who are planning egg freezing may wish to store up to 20 eggs. By undertaking a milder stimulation, and using DuoStim, the woman can store a high number of eggs without risking Ovarian Hyperstimulation Syndrome.
What are the advantages?
The main advantage is the ability to collect a higher number of eggs within a short space of time. This is especially of benefit for women who produce low egg numbers during IVF Stimulation. In many of these women, time is critical.
Duostim avoids what can be excessive delays in between treatment cycles.
At Ballarat IVF, there are significant financial benefits with having a Duostim treatment cycle, compared to two separate IVF stimulation cycles.
What are the disadvantages?
Having two stimulation cycles in a short space of time can be emotionally draining.
There is a small additional risk of infection with a Duostim treatment cycle, and it is not possible to have a fresh embryo transfer with a Duostim cycle.
Whilst the cost of a Duostim cycle is less than two separate cycles, it is more expensive than a single IVF cycle.
What about Egg quality?
Based on Ballarat IVF Experience, the quality of egg collected in the first and second part of a Duostim cycle are the same, with a trend to higher quality eggs being collected in the second part. This is reflected in a small, but not significant increase in pregnancy rates and embryo scores in embryos formed from eggs from ‘second part Duostim’.
On average, about two more eggs are collected from the second part of the Duostim cycle compared with the first.
Do I have a choice?
Yes , based on your discussion with your specialist you may choose a Duostim cycle from the beginningof your treatment cycle.
DuoStim may be suggested by your fertility nurse after your egg collection. The final decision whether to go ahead with this will be made by your Specialist after discussion with you.
There is no compulsion to have a DuoStim treatment cycle. Each woman needs to consider the options, and make a final decision with their Ballarat IVF Fertility Group Specialist.
Percutaneous Epididymal Sperm Aspiration (PESA)
This procedure is used to retrieve sperm from men who have had a vasectomy or other blockage of the vas deferens. A fine needle is placed into the epididymis to aspirate tiny pockets of sperm. This procedure is performed under a light general anaesthetic, but can also be performed under a local anaesthetic.
PESA does not collect enough sperm to achieve a normal conception and so the couple will have to undergo IVF treatment using ICSI. Sperm collected can be frozen for use later.
95% of males undergoing PESA at Ballarat IVF have sperm successfully collected for IVF treatment
Testicular Needle Biopsy (TESA)
This is similar to PESA, but tissue is taken directly from the testicle instead of the epididymis. A general or local anaesthetic is used. A fine needle is used to aspirate tissue from the testis, withdrawing some of the tubules that contain live sperm.
PESA and TESA procedures do not collect enough sperm to achieve a normal conception and so the couple will undergo IVF treatment, in particular using ICSI. Sperm collected using these procedures can be frozen for use later.
Testicular Open Biopsy (TBX)
This procedure is performed when no sperm are present at the time of PESA It requires a general anaesthetic and admission to hospital. A larger amount of testicular tissue is removed.
Dependent on history, this is successful in up to 70% of men who have no sperm in the ejaculate and have no other signs of normal sperm production, and in over 90% of men who have had a previous vasectomy.
Adjuvants (Add-on) treatments
Overall, the likelihood of conceiving with IVF in Australia is about 33% per embryo transfer.
It is stressful, and disappointing when an embryo transfer doesn’t result in a pregnancy.
Most of the time, this due to statistical bad luck, but when a disappointing outcome happens repeatedly, everyone involved asks themselves the question, “Are we missing something?” and “should we do something different in the next treatment cycle?”
Generally speaking, there are two groups of treatment in Assisted reproduction;
- Standard treatments, which are highly likely to influence the likelihood of conceiving, for example, having IVF with blocked fallopian tubes, and using ICSI for couples with profound sperm abnormalities, and
- Adjuvant treatments, which may increase the likelihood of conceiving during IVF treatment. These treatments are usually biologically plausible, and have a level of scientific evidence to support their use in certain patients. Not surprisingly, the levels of plausibility, and the quality of supporting evidence for each adjuvant treatment varies, and based on evolving science, continues to vary. One treatment which seems beneficial, may be shown not to be so with new research, and debate between experts may create further confusion.
Ballarat IVF fertility Specialists are aware of the range to Add On therapies which are available for use, and may influence the outcome of fertility treatment.
Our approach is that if an Adjuvant therapy is biologically plausible, it is safe, there is a reasonable body of supporting evidence, and the therapy is inexpensive, we will discuss it with our patients.
Sometimes our patients ask a question about an adjuvant therapy, and sometimes, we suggest it.
Our patients should feel free to start a conversation about Adjuvant, or Add on therapies. We will provide information to help in the decision-making process.
Locations
Abbreviations have been used throughout this website. Please refer to the glossary for full terminology.
Ballarat IVF acknowledges the Traditional Custodians of the land we live and work on, the Wadawurrung and Dja Dja Wurrung People, and recognises their continuing connection to the land and waterways.
All Rights Reserved | Ballarat IVF
All Rights Reserved | Ballarat IVF
site by mulcahy & co marketing


